
Lung cancer is a huge challenge for modern medicine. It is the most common cancer in the world with a very poor prognosis. In Poland, over 20,000 new cases are diagnosed annually, and around 19,000,000 people die in the same period.
People over 55 are most often affected. The disease is the leading cause of death from cancer in both women and men. It is estimated that by 2035, the disease will cause almost 3 million deaths worldwide.
The most common cancer of this organ is derived from the epithelial cells of the respiratory tract. It can be localized in large bronchi or small bronchioles. Due to its location, it is also called bronchogenic cancer. It develops as a result of abnormal changes in respiratory epithelial cells caused by carcinogens. Other lung cancers, much less common, include lymphomas and non-epithelial cancers.
How does lung cancer manifest?
Symptoms are non-specific, especially in the early stages, and can often be masked by other diseases, e.g. symptoms in smokers can also be caused by chronic obstructive pulmonary disease. It is estimated that even 6-8 months pass from the appearance of the first disturbing symptoms to the diagnosis. Often the disease is diagnosed in radiological examinations performed for other reasons.
Early symptoms of cancer
Due to the very aggressive course, sometimes the first symptoms may result from the emerging metastases, e.g. in the lymph nodes, brain or bones. The occurrence of certain symptoms also depends on the location of the tumor.
Symptoms of lung cancer are very scarce or absent at the beginning. Usually these are:
- cough,
- shortness of breath and wheezing,
- recurrent pulmonary infections,
- hoarseness,
- coughing up secretions with blood,
- chest and shoulder pain,
- increased body temperature,
- feeling tired, weak,
- weight loss not related to dieting.
A symptom that occurs in 45-75% of cough, often accompanied by expectoration of secretions.
In addition, shortness of breath, chest pain, hemoptysis and hoarseness may occur due to damage to the laryngeal nerve. Many patients develop prolonged or recurrent pneumonia.
A tumor located in the upper part of the lung may be responsible for pain in the shoulder that even radiates to the fingers of the hand on the same side. However, if the tumor is located in the central part, it is characterized by the so-called superior vena cava syndrome, causing swelling of the head and neck, and sometimes the upper limbs.
The dissemination of the tumor to the supraclavicular lymph nodes will result in their enlargement. Neurological disorders (headaches, nausea, vomiting, convulsions, paresis, dizziness) are caused by brain metastases, and pathological fractures and bone pain are caused by bone metastases. In addition, the cancer can also spread to the liver, resulting in jaundice, and to the adrenal glands, disrupting the secretion of hormones. Patients may also present with fever, anemia, and weight loss.
Why does lung cancer hurt?
Lung cancer may be pain-free for a very long time. When the pain appears, how intense it will be, and what its nature will be depends on many factors, such as:
- tumor size,
- its location,
- localization of metastases.
Lung cancer usually hurts only when the cancer infiltrates the surrounding tissues or compresses innervated structures in the chest, and when there are metastases to the brain, liver or bones.
Causes of lung cancer
The most important risk factor is active smoking, which is responsible for about 80% of deaths. illnesses. Tobacco smoke contains several thousand chemical compounds, many of which have proven carcinogenic effects, e.g. benzene, vinyl chloride, nitrosopyrrolidine, N-nitrosamines and polycyclic aromatic hydrocarbons. Smoking cigarettes with a lower nicotine content and those that are equipped with filters is also very harmful and does not protect against the development of cancer. Smoking a pipe or cigar also has a similar effect.
In addition, in the pathogenesis of this disease, the length of time of smoking, the number of cigarettes smoked, and the age at which smoking was started are important. There is also an increased risk of disease in passive smokers, i.e. people who do not smoke, but are exposed to the harmful effects of tobacco smoke. Giving up the addiction gradually reduces the risk of the disease, but it is never at such a low level as in non-smokers.
Other causes include environmental and occupational factors. They include e.g. ionizing radiation, exposure to asbestos, cadmium, radon, beryllium, nickel, silica and vinyl chloride. Air pollution also plays an important role.
The importance of genetic factors in the development of lung cancer is not yet sufficiently understood. It has been established that people with a family history of lung cancer are twice as likely to develop the disease. It is assumed that the tendency to slow DNA repair may be inherited, as well as increased susceptibility to the harmful effects of carcinogenic components of tobacco smoke. As a rule, the tendency to smoke tobacco runs in the family, and the presence of a smoking person in the family results in exposure to passive smoking of other family members. It has not yet been determined whether the increased risk of lung cancer in this population group is due to exposure to cigarette smoke or whether genetic factors are responsible.
It has been observed that HIV-infected people are twice as likely to get sick. This may be due to impaired immunity and smoking itself, which is at a high level in this population group.
Lung cancer diagnosis
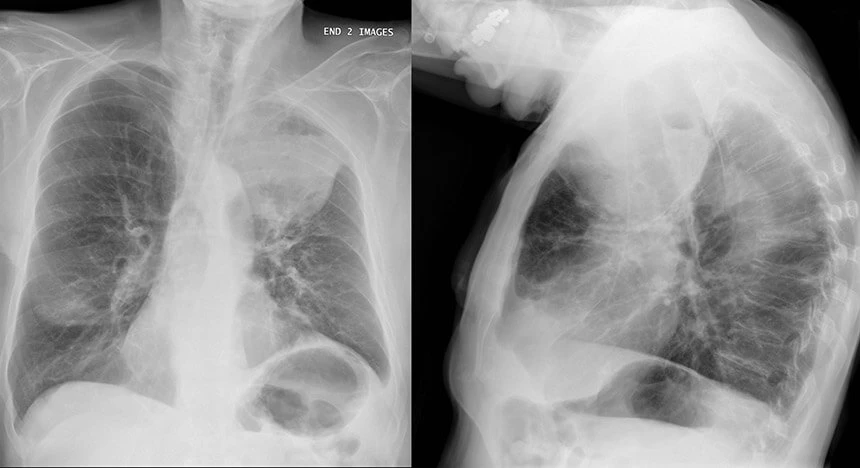
Lung cancer is usually diagnosed when the disease is very advanced. When the disease is suspected, an interview with the patient, as well as physical and imaging tests are important.
Endoscopic examination of the bronchial tree, such as bronchoscopy or endoscopic ultrasound examinations, is used for diagnosis. The final diagnosis, however, is made on the basis of a microscopic examination, most often performed with the use of a fine- or thick-needle biopsy of the lymph nodes (using bronchoscopy) or a biopsy of metastases located outside the chest.
Sometimes a biopsy is needed after chest opening surgery. In the case of tumors located in the central part of the lung, it is possible to perform a respiratory secretion test.
Sputum examination may also be helpful in the diagnosis, both for tuberculosis and for a detailed assessment of the likelihood of the presence of suspicious cells from the bronchial tree.
Once diagnosed with lung cancer, it is very important to determine how advanced the cancer is and to detect any metastases. Physical and imaging tests are used for this purpose, e.g. chest X-ray, ultrasound, computed tomography, magnetic resonance imaging, bone scintigraphy.
Positron emission tomography (PET) is recommended in some patients. In addition, in some cases it is important to bronchoscopy or videothoracoscopy.
Lung cancer marker
The CYFRA 21-1 and NSE tumor markers are used to diagnose non-small cell lung cancer. In cancer, an increase in the concentration of the SCC-Ag marker is also observed.
Histological types of lung cancer
Due to the different clinical picture and different therapeutic possibilities, lung cancer is divided into two categories: small-cell carcinoma (SCLC) and non-small-cell carcinoma (NSCLC), to which include: squamous, glandular and large cell.
Small cell carcinoma
It accounts for about 20 percent. all cases of lung cancer. It is characterized by a very aggressive course and fast growth. In the early phase of the disease, the cancer spreads. Metastases are usually located in the bones, skin, bone marrow, lymph nodes and brain. It most often involves the large bronchi. This is the type of cancer that shows the strongest association with nicotine smoking.
Anti-Ri antibodies are sometimes found before the onset of symptoms of this type of cancer. Check when onconeural antibody testing is indicated.
Although it is highly sensitive to radio- and chemotherapy, the prognosis is poor. Distant metastases are usually present at the time of diagnosis. In the course of this type of cancer, there are often paraneoplastic symptoms, which include neurological and endocrine disorders, skin complaints (e.g. lupus symptoms, dermatomyositis, clubbing). In addition, thromboembolic complications, electrolyte disturbances and anemia may occur.
Squamous cell carcinoma
It accounts for about 40-50 percent. primary lung cancers. It is more common in the elderly. Men are more prone to the disease. It is also associated with smoking. It is usually centrally located. It is characterized by slow development. It is most often preceded by precancerous conditions related to changes in the appearance and dysfunction of the respiratory epithelium.
Adenocarcinoma
Diagnosed in about 35 percent. patients with primary lung cancer. It is much more common in women. It is diagnosed in non-smokers, therefore exposure to tobacco smoke is of little importance in its pathogenesis. The tumor is usually located in the peripheral parts of the lungs. It is characterized by slow growth, but due to its rich vascularity, it quickly metastasizes, most often to the brain. In recent decades, an increased incidence of this type of lung cancer has been observed.
Large cell carcinoma
It accounts for about 10 percent. all primary lung cancers. It is made of large cells. It can be localized both in the central parts of the lungs, as well as in the peripheral ones. It is characterized by rapid growth and dissemination to distant organs.
Stages of lung cancer (metastasis)
In assessing the prognosis and choosing the best treatment, it is also important to determine the stage of the disease. The TNM classification developed by the International Association for the Study of LungCancer is used for this purpose.
The feature T (tumor) defines the size of the tumor, N (node) – the presence of metastases to the regional lymph nodes of the chest, and M (metastases) – the appearance of distant metastases.
Based on the assessment of the tumor, the following stages of neoplastic disease are distinguished:
- I degree – the tumor is limited only to the lung parenchyma, no metastases in regional lymph nodes, the tumor does not infiltrate the structures of the mediastinum;
- II degree – cancer limited to the lung parenchyma, presence of metastases in the lymph nodes of the lung hilum;
- III degree - the tumor infiltrates the mediastinal structures, chest, spine or there are metastases in the mediastinal or supraclavicular lymph nodes;
- IV degree – distant metastases (brain, adrenal glands, bones, liver) or dissemination to the pleural cavity.
What metastases does lung cancer give?
In the course of lung cancer, metastases to distant organs often occur. Due to the fact that lung cancer is often diagnosed at an advanced stage, approximately 40% of newly detected cases are associated with already existing metastases. They are most often attacked:
- liver
- brain
- bones
- the adrenal glands
Liver metastases are generally associated with the worst prognosis of all lung cancer complications.
Metastases to the central nervous system are also one of the most serious complications of this disease. Although there are no global data on the incidence of metastases, conservative estimates suggest that 10 to 30% of patients diagnosed with lung cancer may develop brain metastases.
Bone metastases are a common complication. The spine, pelvis and ribs are most commonly affected.
Primary adrenal tumors are very rare. Adrenal cancer is usually a metastasis of another organ, including a malignant tumor of the lungs.
Treatment of tumors that are metastases of lung cancer consists primarily of therapy aimed at removing the primary lesion, i.e. lung cancer. Metastatic neoplastic lesions, depending on the location, may be surgically removed.
Treatment of lung cancer
Despite the development of medicine and pharmacotherapy, therapeutic possibilities in the case of lung cancer are not satisfactory. The chance of being cured and surviving at least 5 years is less than 10-15%. people diagnosed with cancer. Annual mortality is close to the number of new diagnosed cases. The choice of appropriate treatment depends on the stage of the disease, the presence of comorbidities, and the efficiency of the patient's body.
Surgical treatment
In the case of local or regional cancer, surgical methods are usually chosen, consisting in resection of the tumor with a margin of safety. Often it is necessary to remove the entire lobe of the lung. Surgical treatment is most often supported by chemotherapy.
When is lung cancer inoperable?
Often, however, surgical treatment is not possible. Surgery may be ruled out due to some comorbidities. This method is usually not applicable in stage III/IV disease. Occasionally, a surgeon may decide to surgically remove a stage IIIA tumor, provided that complete excision is possible.
A tumor is also inoperable when its location poses a risk of damaging adjacent, important anatomical structures during surgery.
Chemotherapy, radiotherapy, palliative treatment
Chemotherapy is also the main treatment for small cell carcinoma. Patients who are not eligible for surgery should receive radiotherapy. Sometimes combined treatment is recommended, consisting of a combination of radiotherapy and chemotherapy, and sometimes surgery. A small group of patients with non-small cell lung cancer is eligible for targeted molecular therapy. Unfortunately, many patients have dissemination to distant organs at the time of diagnosis. These people receive palliative treatment (i.e. symptomatic treatment), in some cases supported by radio- or chemotherapy. It is aimed at prolonging the patient's life and maintaining its relatively good quality. It is also extremely important to conduct psychological counseling in this group of patients.
Systemic anticancer treatment, selected individually depending on the expression of receptors and proteins characteristic of a given tumor, is very effective.
Lung cancer - what are the chances of survival? Prognosis
Lung cancer is one of the worst malignant tumors. Due to the lack of specific symptoms, the disease is usually diagnosed at an advanced stage, when therapeutic options are very limited. In addition, older people are much more likely to get sick. More than half of the patients are over 65 years of age, and age is a factor significantly worsening the prognosis.
In addition, the effectiveness of therapy is affected by the general condition of the patient and the presence of comorbidities. Only about 10% have a chance of being cured and have a 5-year survival rate. sick. The vast majority, despite treatment, die within 2 years of diagnosis. If distant metastases are present at the time of diagnosis and no treatment is undertaken, then survival is usually 6–8 weeks.
Complications of lung cancer
Patients with this cancer are burdened with numerous complications. They are caused by the growth of the tumor, and may also be the result of the treatment used (chemotherapy, radiotherapy). In addition to pain, patients experience metabolic and electrolyte disorders, peripheral neuropathies, respiratory problems, weakness and loss of appetite leading even to malnutrition. In addition, patients often experience anxiety disorders, insomnia and even depression.
How fast does lung cancer progress?
The rate of tumor growth depends on the histological type of the tumor. Small cell carcinoma develops the fastest, and without treatment it can lead to the patient's death within a few months of diagnosis. Non-small cell carcinoma, responsible for the vast majority of lung cancer cases, develops much more slowly.
In addition, a number of factors affect the rate at which lung cancer develops. Smokers have a faster increase in tumor size than non-smokers. In the case of inoperable tumors, the development of lesions is often slowed down or stopped as a result of the applied treatment (mainly chemotherapy and radiotherapy).
Lung cancer prevention
There are currently no screening studies. Chest X-rays or sputum cytology may help to diagnose the disease at an earlier stage, but they do not reduce mortality.
The most effective and the cheapest method to reduce lung cancer morbidity and mortality is cessation of active and passive smoking. Smoking 20 cigarettes a day increases the risk of getting sick by about 25%, and 40 cigarettes by 60%. Giving up the addiction is associated with a gradual decrease in the incidence of this cancer. After about 15 years, a former smoker's risk of developing the disease is reduced by almost 80%. It is extremely important to carry out preventive actions aimed at making the society aware of the harmful effects of tobacco smoke. Of great importance is counseling aimed at persuading patients to stop smoking tobacco, pipes and marijuana, as well as pharmacological support under the supervision of the attending physician, aimed at reducing the symptoms of nicotine craving.
Other important aspects in the development of lung cancer are occupational and environmental factors. Research is constantly being conducted on the negative impact of ionizing radiation, as well as occupational exposure, e.g. to nickel, asbestos or cadmium. In addition, it has been observed that higher levels of air pollution increase the incidence of lung cancer. It is very important to develop new or clarify the existing regulations to protect employees from the harmful effects of carcinogenic substances in the workplace. It is also important to take action to reduce the pollution of the environment in which we live.
Diet is also believed to be a factor modifying the risk of developing the disease. Research is still ongoing on the consumption of vegetables and fruits, rich in antioxidant substances that can protect DNA from damage caused, for example, by carcinogenic components of tobacco smoke. No benefits of vitamin A or E supplementation have been observed.
Physical activity and maintaining a healthy body weight may also be responsible for a reduced incidence of lung cancer. A factor that may increase the risk of this disease is excessive alcohol consumption, especially when combined with exposure to tobacco smoke. Leading a healthy lifestyle is of great importance in the prevention of many diseases and can also contribute to reducing the number of diseases.
Lung cancer prevention program of the Ministry of Health
The Ministry of Health has introduced a National Program for Early Detection of Lung Cancer using Low-Dose Computed Tomography for people at particular risk of the disease. The campaign includes people from risk groups.
Sources:
Modlińska A., Kowalczyk A. „Rak płuca – epidemiologia, obraz kliniczny oraz społeczne następstwa choroby.” Psychoonkologia 2016 20 (2): 57– 65.
Pawlicka M., Mroczek A. , Bałabuszek K., Radzka A., Fałkowska U. „ Rak płuc: epidemiologia, profilaktyka i leczenie.” Nauki Przyrodnicze i Medyczne: Postępy w farmakologii i onkologii, Lublin 2018 97–109.
- Rak płuca • Nowa Medycyna 3/2003 • Czytelnia Medyczna BORGIS dostęp dnia 07.07.2022
- Szlitkus P. „Epidemiologia nowotworu płuc w Polsce.” Zeszyty Naukowe WCO, Letters in Oncology Science 2018;15(2):71-77.
- Lung cancer epidemiology: contemporary and future challenges worldwide - PMC (nih.gov) dostęp dnia 07.07.2022
- Płuco i opłucna | KRN (onkologia.org.pl) dostęp dnia 07.07.2022
- Starek A. , Podolak I. „Rakotwórcze działanie dymu tytoniowego.” ROCZN. PZH 2009, 60, Nr 4, 299 – 310.
- Rzyman W. „Rak płuca.” Forum Medycyny Rodzinnej 2008, tom 2, nr 6, 407–419.
- cdc.gov./cancer/lung/basic_info/risk_factors.htm dostęp z dnia 07.07.2022
- cancer.gov/types/lung/patient/lung-prevention-pdq dostęp dnia 07.07.2022
- Program profilaktyki raka płuca | Pacjent
- Sperduto PW, Yang TJ, Beal K, et al. Estimating Survival in Patients With Lung Cancer and Brain Metastases: An Update of the Graded Prognostic Assessment for Lung Cancer Using Molecular Markers (Lung-molGPA). JAMA Oncol. 2017;3(6):827–831. doi:10.1001/jamaoncol.2016.3834
- Ren Y, Dai C, Zheng H, Zhou F, She Y, Jiang G, Fei K, Yang P, Xie D, Chen C. Prognostic effect of liver metastasis in lung cancer patients with distant metastasis. Oncotarget. 2016 Aug 16;7(33):53245-53253. doi: 10.18632/oncotarget.10644. PMID: 27449299; PMCID: PMC5288182.
| The presented medical information should not be treated as guidelines for medical conduct in relation to each patient. The medical procedure, including the scope and frequency of diagnostic tests and/or therapeutic procedures, is decided by the doctor individually, in accordance with medical indications, which he determines after getting acquainted with the patient's condition. The doctor makes the decision in consultation with the patient. If the patient wants to perform tests not covered by medical indications, the patient has the option of paying for them. |
Prezentowanych informacji o charakterze medycznym nie należy traktować jako wytycznych postępowania medycznego w stosunku do każdego pacjenta. O postępowaniu medycznym, w tym o zakresie i częstotliwości badań diagnostycznych i/lub procedur terapeutycznych decyduje lekarz indywidualnie, zgodnie ze wskazaniami medycznymi, które ustala po zapoznaniu się ze stanem pacjenta. Lekarz podejmuje decyzję w porozumieniu z pacjentem. W przypadku chęci realizacji badań nieobjętych wskazaniami lekarskimi, pacjent ma możliwość ich odpłatnego wykonania. Należy potwierdzić przy zakupie badania szczegóły do jego przygotowania. |
