Genetic Predisposition Screening
for colorectal cancer. BUY

Colorectal cancer epidemiology
It is the second malignant tumor in Poland in terms of the cause of death. Both incidence and mortality continue to increase.
In 2013, over 17,000 were recorded in Poland. cases of colorectal cancer, and 11 thousand. people died from colorectal cancer. This cancer rarely affects people before the age of 40, but after crossing this border, the risk of developing the disease increases and reaches its peak in the eighth decade of life.
Colon cancer symptoms
Symptoms of colorectal cancer vary depending on the stage and location of the tumor. In right bowel cancer, the symptom is usually occult bleeding with progressive anemia. When the cancer is located on the left side, the most common symptom is overt bleeding from the lower gastrointestinal tract and a change in bowel habits.
How does colorectal cancer hurt? – this is quite often a question asked by patients. Bowel cancer is usually painless, which may be why many patients see their doctor too late.
Common early symptoms of colorectal cancer:
- rectal bleeding
- the presence of blood in the stool
- anemia (comes from small, often hidden, but constant bleeding from the tumor into the lumen of the large intestine)
- alternation of diarrhea and constipation or persistent diarrhea
- change in the shape and size of the stool (the so-called "pencil-like" stools) - this weighs on the symptom reported by patients
- abdominal pain
- constant pressure to stool
Later, the symptoms of colorectal cancer are joined by the classic symptoms of advanced cancer: progressive weight loss, lack of appetite and weakness.
If you notice any of the symptoms listed above, contact your doctor.
Causes of colorectal cancer
The formation and development of cancer have many causes, but the most important are genetic and environmental factors.
Genetic factors are the main cause of approximately 15-30% of all cases of the disease. These include:
- Lynch syndrome, formerly called hereditary colorectal cancer not related to polyposis - it is the most common cause of genetically determined colorectal cancer and accounts for 1-3% of cases of this cancer
- previous history of colorectal cancer or excision of polyps1 with a high degree of dysplasia2
- a family history of colorectal cancer
- familial adenomatous polyposis syndrome3, which is considered to be the so-called precancerous condition
- inflammatory bowel diseases (Crohn's disease4 increases the risk 3-fold, ulcerative colitis 20-fold)
Environmental risk factors for the development of colorectal cancer are associated with the majority of cases. Belong to them:
- age >50. years
- obesity
- smoking cigarettes (in the USA, 20% of colorectal cancers are related to smoking)
- low physical activity
- a diet that promotes constipation and adversely affects the bacterial flora of the intestines, causes the formation of carcinogenic compounds and extends their transit time through the large intestine:
o poor in fruits and vegetables as well as calcium, fiber and selenium
o Rich in animal fats and high in calories
- previous radiotherapy of the abdominal cavity
- taking immunosuppressants after an organ transplant
And a little less often:
- alcohol abuse
- previous cholecystectomy
- HPV infections
- a history of cervical, vulvar or vaginal cancer
Diagnosis of colorectal cancer
Reliable and unambiguous diagnosis is possible only in the histopathological examination of specimens taken from the lesion (e.g. from a tumor, polyp or mucosa) or the entire removed fragment. This examination, in addition to the diagnosis itself, can provide information about the type of cancer, which in turn determines the planning of the appropriate treatment process.
There are many tests that allow you to confirm the presence of a suspicious lesion in the intestine and assess whether it should be examined histopathologically.
- Stool occult blood test – this checks if there is blood in the stool that cannot be seen with the naked eye. It is used as a screening test for colorectal cancer.
- Rectal examination (in front of the anus) - the doctor inserts a finger into the anus and palpates the lower part of the rectum. In this way, the presence of changes in the anus, anal canal and the end of the rectum (6-10 cm) can be detected.
- Rectoscopy - viewing the end of the rectum (approximately 30 cm of the end) through a special speculum. It allows to determine the presence of changes in this section of the large intestine and, if necessary, to collect biopsies for histopathological examination. Sometimes it is also possible to remove small polyps1.
- Colonoscopy – examination performed with a long (approx. 150-180 cm), flexible endoscope inserted through the anus. Thanks to it, you can assess the lumen of the intestine, view the entire large intestine, up to the place where it connects to the small intestine. Samples for histopathological examination or removal of small polyps can be taken during colonoscopy if needed1. The condition for the success of the endoscopic examination is proper preparation, in accordance with the instructions of the referring physician.
- Contrast infusion - currently rarely performed. It consists in injecting air into the large intestine and administering a contrast agent and taking a series of X-ray images of the abdominal cavity, which show the outline of the intestinal wall. Based on this, the presence of suspicious changes in the intestinal wall can be determined. This examination is less accurate than colonoscopy and during its performance no biopsies can be taken for histopathological examination.
- Virtual colonoscopy (colonography) – the examination consists in creating a three-dimensional image of the large intestine thanks to a series of images taken with a computer tomograph. As in the case of traditional colonoscopy, the condition for the success of virtual colonoscopy is proper preparation for the examination, in accordance with the instructions of the referring physician. To perform this test, intravenous administration of a special contrast is needed, and the interpretation of images is sometimes ambiguous - all this makes virtual colonoscopy not performed very often. An additional limitation of this method is the inability to remove any changes or collect them for microscopic examination.
- Testing the concentration of the marker5 CEA (carcinoembryonic antigen) in the blood – this antigen6 is a marker whose elevated level is observed in patients with colorectal cancer. CEA determination is most often used to monitor the condition of patients after cancer treatment in order to observe whether the disease has not recurred.
Treatment of colorectal cancer
The main method of treating colorectal cancer is surgery. However, before it happens, it is necessary to perform a number of additional tests, such as ultrasound or computed tomography. They will allow doctors to determine whether surgery is possible, and if so, what kind of surgery to choose. Based on these tests, they will also determine if any additional treatment is needed before surgery.
In the case of advanced neoplastic changes involving the lymph nodes of the abdominal cavity and pelvis, therapy is necessary before the procedure - radiotherapy and treatment with anticancer drugs (so-called neoadjuvent therapy).
Depending on the size of the tumor and its location, the lesion is removed together with an appropriate fragment of a healthy intestine and, usually, nearby lymph nodes. Often, during the operation, it is possible to stitch (anastomose) the remaining parts of the intestine, thanks to which the operation is not associated with deterioration of the quality of life for these patients.
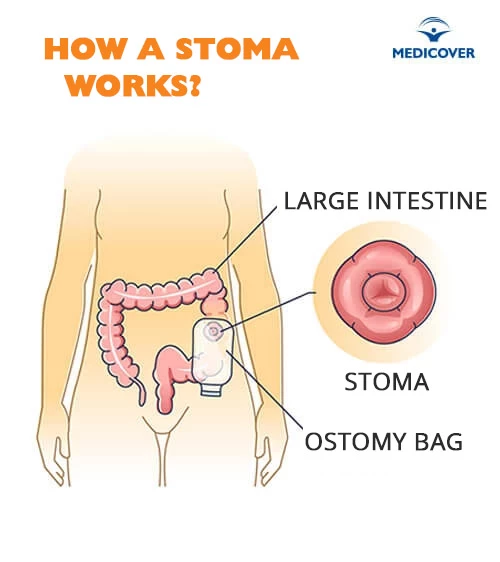
Stoma
It happens, however, that this stitching is not possible - then the so-called "artificial anus", or stoma. It is an opening in the abdominal wall, to which the final section of the large intestine is led on one side, and a plastic reservoir, called an ostomy bag, on the other. Stool is excreted into this bag. The stoma may be created for some time, e.g. until the anastomosis heals, or forever.
Multi-organ surgery
When the cancer is at a very advanced stage and has invaded neighboring organs (e.g. stomach, liver, spleen, kidney, abdominal wall, bladder or ovary), multi-organ surgery may be necessary. It consists in excision of the primary tumor together with a fragment of the intestine and part or all of the affected organs. In such cases, it often turns out that the extent and localization of the lesions make it impossible to perform a proper operation and complementary treatment, e.g. chemotherapy, is necessary.
Control after surgery
After complete excision of the tumor, patients are checked every 2-3 months for the first 2 years, then less often, until the 5th year after surgery. Monitoring of their condition is based on blood levels of the CEA marker5 every 3 months for 3 years, abdominal tomography or ultrasound and chest X-ray every year, and a full colonoscopy in approximately 6 months, 3 years and 5 years after surgery.
Prognosis and complications of colorectal cancer
The prognosis for colorectal cancer, as with other cancers, depends on the stage of the tumor at the time of diagnosis. Due to the fact that almost 80% of colorectal cancers are diagnosed in late stages, the 5-year survival rate is about 40%. If metastases occur, 25-35% of patients survive 5 years after their complete excision.
Colorectal cancer metastases
A complication of colorectal cancer may be the occurrence of metastases throughout the body. They are a symptom of the advancement of the disease and reduce the chance of a full recovery. Through blood vessels and lymph vessels, cancer most often attacks the liver, less often the lungs, ovaries, adrenal glands, brain and bones.
Colorectal cancer prevention
In people who are not in the risk group, actions that reduce the risk of developing cancer include:
- regular physical activity
- taking care of a proper diet - limiting fats (especially those of animal origin), daily consumption of fresh fruit and vegetables, reducing the caloric content of meals, limiting alcohol consumption
- regular screening after the age of 50
- about a colonoscopy every 10 years or
- testing for fecal occult blood every 2 years
If genetic tests show that we have a gene mutation responsible for the development of the disease, it does not mean that we are doomed to this disease. It only means that the risk of getting sick is much higher for us than for others.
In people with genetic predisposition to the development of colorectal cancer, prophylaxis is tailored individually and is based on more frequent prophylactic colonoscopy examinations and starting them at a younger age.
Remember!
- Quit smoking and reduce alcohol consumption.
- Take care of a proper diet.
- Avoid constipation.
- Be physically active on a regular basis.
- Maintain a healthy weight.
- Get preventive examinations. If you notice disturbing symptoms, contact your doctor!
Prevention
|
The presented medical information should not be treated as guidelines for medical conduct in relation to each patient. The medical procedure, including the scope and frequency of diagnostic tests and/or therapeutic procedures, is decided by the doctor individually, in accordance with medical indications, which he determines after getting acquainted with the patient's condition. The doctor makes the decision in consultation with the patient. If the patient wants to perform tests not covered by medical indications, the patient has the option of paying for them. |
Prezentowanych informacji o charakterze medycznym nie należy traktować jako wytycznych postępowania medycznego w stosunku do każdego pacjenta. O postępowaniu medycznym, w tym o zakresie i częstotliwości badań diagnostycznych i/lub procedur terapeutycznych decyduje lekarz indywidualnie, zgodnie ze wskazaniami medycznymi, które ustala po zapoznaniu się ze stanem pacjenta. Lekarz podejmuje decyzję w porozumieniu z pacjentem. W przypadku chęci realizacji badań nieobjętych wskazaniami lekarskimi, pacjent ma możliwość ich odpłatnego wykonania. Należy potwierdzić przy zakupie badania szczegóły do jego przygotowania. |
