Melanoma - general information
Epidemiology:
Melanoma is one of the most malignant tumors. It originates from melanocytes, i.e. pigment cells, skin or mucous membranes (e.g. vulva, anus, mouth) or from the vascular membrane of the eyeball. The incidence of this cancer is about 5-7 percent. all skin cancers. The incidence of melanoma is highest among Caucasians due to the fair skin phenotype (fair complexion, light hair and eye color, freckles, easy sunburn).
Melanoma incidence - statistics:
Most patients are recorded in Australia - there are much fewer of them in Poland, but the number is growing rapidly. This increase is associated with a change in lifestyle and the fashion for sunbathing and causes that melanoma is increasingly diagnosed in young people, even in their 20s and 30s.
Melanoma symptoms
The symptoms of melanoma depend on the degree of its development. In the early form, the lesions are flat, asymmetric, with a non-uniform color and irregular, jagged edges. In the advanced form, the lesions are often raised above the skin level, and sometimes also ulcerated with oozing blood-tinged secretions. In some situations, such as anal or subungual melanoma, the first symptom of the disease may be enlarged lymph nodes in the area where the disease develops.
Other skin cancers:
- Basal cell carcinoma
- Squamous cell carcinoma
Moles what to watch out for?
Virtually everyone has from a few to even several hundred moles and other birthmarks on their skin. Some like them, others don't, but it's not the aesthetic dimension that matters here. They should also be assessed in terms of health.
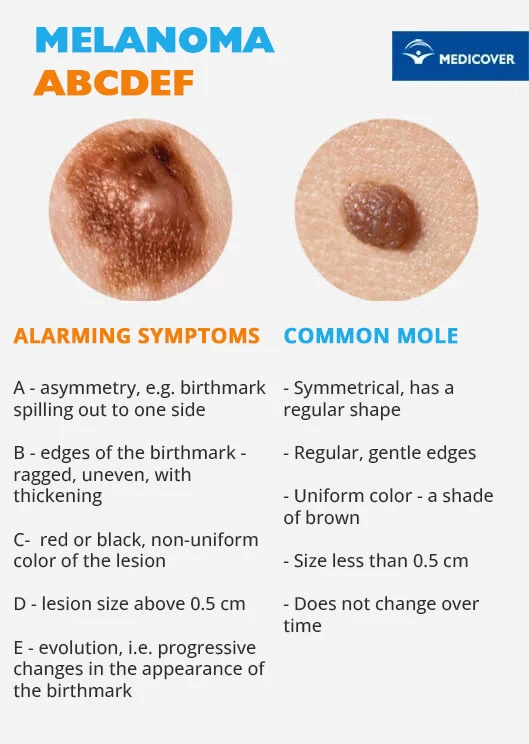
We should be concerned primarily with: irregular shape, uneven edges, uneven color, size over 5 mm, as well as itching or changes in shape or size. These may be signs of developing melanoma.
This cancer originates from melanocytes, i.e. pigment cells that produce and contain melanin, which can be malignantly mutated. Melanoma most commonly occurs on the skin, but can also appear anywhere melanocytes are present. For example, on the mucous membranes or in the retina of the eye.
What does melanoma look like?

Ultraviolet (UV) radiation plays an important role in the formation of this cancer. It has a direct effect on the genetic material of epidermal cells, leading to its damage and weakening the repair processes of the skin. This action is harmful to everyone, but some people are at exceptional risk of developing melanoma. This group includes:
- carriers of specific gene mutations,
- people whose close family has been diagnosed with melanoma,
- people suffering from melanoma or other malignant skin tumors in the past,
- people who have numerous (>50) pigmented moles1, atypical or changeable moles,
- people with light skin, light or red hair, blue eyes and freckles,
- people who periodically and intensively expose themselves to UV radiation, e.g. sunbathe in the sun or in a solarium,
- people prone to sunburn,
- people who have suffered severe sunburn in childhood or adolescence,
- immunocompromised people, eg patients taking immunosuppressants after an organ transplant.
Melanoma risk factors
Melanomas are most common in middle-aged people and are especially dangerous for fair-skinned people. The high-risk group also includes people who were constantly exposed to solar radiation or burns as a child. This cancer also threatens people with congenital pigmented moles and a large number of even small moles.
According to statistics, it is more common in women, but the course of the disease is much more severe in men. This cancer can run in families, and the risk of developing melanoma increases the more relatives have had the disease. The likelihood of its development increases exposure to ultraviolet radiation from the sun or artificial sources, such as, for example, a tanning bed.
Early detection of melanoma allows for its quick treatment. What are the symptoms and diagnosis in patients with this type of skin cancer.
Diagnosis of melanoma
The basis for detecting this cancer is a thorough medical examination of the entire skin, in particular the scalp, hands, feet and spaces between the toes. Features of a skin lesion that may suggest melanoma include:
- asymmetrical, irregular shape,
- non-uniform color,
- uneven, ragged edges,
- changes in shape and size,
- size above 5 mm, dynamics of changes in appearance,
- itching, bleeding, ulceration.
Histopathological examination of the entire surgically removed lesion is necessary to confirm the diagnosis, staging and prognosis. The suspicious lesion is excised in its entirety with a margin of healthy skin and sent for histopathological examination. This procedure is called an excisional biopsy. If the suspicion of this tumor is confirmed, depending on the result obtained and the assessment of the margins of the excised lesion, in some patients it is necessary to excision the scar after the removal of the primary lesion.
In addition, in some patients, the doctor may decide to perform a sentinel lymph node biopsy - i.e. the one that is the first on the path of lymph drainage from the area of the excised melanoma. Basic laboratory tests are also performed as standard, e.g. assessment of lactate dehydrogenase (LDH) concentration, chest x-ray and abdominal ultrasound.
Degrees:
|
Methods of treating melanoma
As with any cancer, the most important role in the treatment of melanoma is its early detection. Each disturbing birthmark requires a dermatological consultation. Although only a part of melanomas, about 40%, develops from pre-existing nevi, and the rest develops on unchanged skin, regular dermatological control of the skin is the basis for quick detection and thus effective treatment.
The cornerstone of melanoma treatment is surgical treatment, which consists in excision of the lesion with a margin of healthy skin. After confirmation of melanoma in histopathological examination, a decision may be made to excise the scar with appropriate margins and to perform a sentinel node biopsy. A sentinel node is a lymph node that is the first on the path of lymph drainage from the area of the excised melanoma. If a metastasis is found in the sentinel node, lymph nodes are removed from the entire lymph drainage area, i.e. the so-called lymphadenectomy.
In the advanced stages of this cancer, the management is individualized. The methods of treatment used include: surgery, radiotherapy, chemotherapy, immunotherapy2 and targeted treatment - molecularly targeted.
Check out Medicover's cancer treatment offer >>
Melanoma - prognosis and complications
Melanomas developing on the limbs have a better prognosis than on the trunk. The risk of recurrence increases with the depth of infiltration of the primary lesion. The highest probability of recurrence occurs in the first 2-3 years after treatment. During this period, there is an increased intensity of medical check-ups. Depending on the stage and primary location of melanoma, the risk of local recurrence ranges from 3 to 15%.
Less than 5% of patients have relapsed 5 years after treatment. sick. Melanoma metastases can occur via lymph and blood vessels. Their appearance is associated with a greater advancement of the disease and worsens the prognosis. In the early stages of melanoma, the cure rate is 90-10%.
After treatment, regular check-ups are recommended as recommended by your doctor.
Melanoma prevention
Prevention of advanced melanoma is based on:
- assessing each patient's risk characteristics and adjusting prophylactic procedures,
- providing people from risk groups with more detailed care,
- avoiding excessive exposure to the sun, especially short episodes of intense sunlight causing skin burns,
- avoiding tanning in solariums,
- taking care of adequate protection against the sun, using creams with a UV filter,
- regular observation and assessment of moles according to the ABCDE principle.
Remember:
- Watch your skin and moles every month, and if something concerns you, contact a dermatologist.
- Check your skin and moles once a year at a doctor's appointment.
- Take care of adequate sun protection - use creams with a high UV filter, avoid exposing yourself to the sun between 10.00 and 16.00, wear sunglasses with a UV filter.
Melanoma prevention - research
Although for many of us the diagnosis of "melanoma" may sound like a sentence, doctors emphasize that this disease does not have to be incurable or even fatal. However, there is a condition. Early-detected melanomas have a very high cure rate. When the lesion is 1-2 mm thick, it is 80-90 percent. So, to increase your chances, you need to remember to have moles checked by a dermatologist once a year.
The most modern method of diagnosis is videodermoscopy (also called videodermatoscopy) - it is a completely non-invasive method that allows you to assess skin changes under magnification, as well as save their image in electronic form. If at this stage something concerns the doctor, a histopathological examination of the suspicious lesion is performed, cutting it out in its entirety along with a margin of healthy skin and submitting it for examination. In the early stages, treatment can usually be stopped at this point. If the cancer is more advanced, chemotherapy and immunotherapy are used.
Check out Medicover's cancer prevention offer >>
See how videodermoscopy looks like:
Sources:
- „Interna Szczeklika 2015”.
- „Podstawy chirurgii” wyd. Medycyna Praktyczna.
- „Nowotwory skóry: klinika, patologia, leczenie” A. Bieniek, M. Cisło, A. Jankowska-Konsur.
- „Czerniaki skóry – zasady postępowania diagnostyczno-terapeutycznego” Przegląd Dermatologiczny, 2009, 96, str. 193-203.
- https://www.dermatologia-praktyczna.pl/a1623/Czerniak-----najczesciej-wystepujacy-nowotwor-zlosliwy-skory.html
- https://www.onkonet.pl/dp_czerniakzs2.php#menu7
Footnotes:
1 Dysplastic nevus syndrome is genetically determined. It is found in people with very numerous atypical moles (from 10 to over 100). They occur on the skin of the whole body, but the most dangerous are those on exposed skin (e.g. hands) and hairy scalp.
2 A general term for a set of therapeutic methods consisting in changing the functioning of the immune system (e.g. immunosuppression inhibits its activity, and immunostimulation stimulates it). Immunotherapy is used in in the treatment of cancer, autoimmune diseases and in transplantology.
Medicover offer
|
The presented medical information should not be treated as guidelines for medical conduct in relation to each patient. The medical procedure, including the scope and frequency of diagnostic tests and/or therapeutic procedures, is decided by the doctor individually, in accordance with medical indications, which he determines after getting acquainted with the patient's condition. The doctor makes the decision in consultation with the patient. If the patient wants to perform tests not covered by medical indications, the patient has the option of paying for them. |
Prezentowanych informacji o charakterze medycznym nie należy traktować jako wytycznych postępowania medycznego w stosunku do każdego pacjenta. O postępowaniu medycznym, w tym o zakresie i częstotliwości badań diagnostycznych i/lub procedur terapeutycznych decyduje lekarz indywidualnie, zgodnie ze wskazaniami medycznymi, które ustala po zapoznaniu się ze stanem pacjenta. Lekarz podejmuje decyzję w porozumieniu z pacjentem. W przypadku chęci realizacji badań nieobjętych wskazaniami lekarskimi, pacjent ma możliwość ich odpłatnego wykonania. Należy potwierdzić przy zakupie badania szczegóły do jego przygotowania. |

