The risk of developing many cancers is due to the interaction of inherited gene variants and environmental factors, including chemical, physical and infectious factors, as well as behavioral or nutritional factors. Genetic testing helps prevent these diseases, including by promoting health in people who are at high risk of developing the disease due to mutations in their genetic material (DNA).
Table of Contents:
- Is cancer a genetic disease?
- Is cancer hereditary?
- Genetic counseling and testing
- Should everyone get genetic testing to determine their cancer risk?
- What genetic tests for cancer are currently being performed?
- Genetic testing for breast and ovarian cancer
- Genetic testing for prostate cancer
- Genetic testing for colorectal cancer
- Genetic testing and HPV
- Summary
Human health depends on many different factors: from lifestyle factors such as diet or smoking, to environmental factors and the quality of healthcare. Genetic factors, i.e. changes in the genetic material (mutations), also affect health, e.g. increase the likelihood of developing cancer. This genetic load can be determined by genetic testing. The detection of mutations can provide clues about the types of diseases to which we are susceptible.
Is cancer a genetic disease?
Yes, cancer is a genetic disease caused by changes (mutations) in DNA (genes) resulting from errors in replication or environmental factors: physical, chemical or biological. Genes are segments of DNA that contain instructions for making a protein or several proteins. This determines not only the structure of the body, i.e. how we look, but also its functioning, including the predisposition to the development of diseases.
Each cell of an organism/body contains a copy of genes that act as instructions. Genes control how cells grow and reproduce.
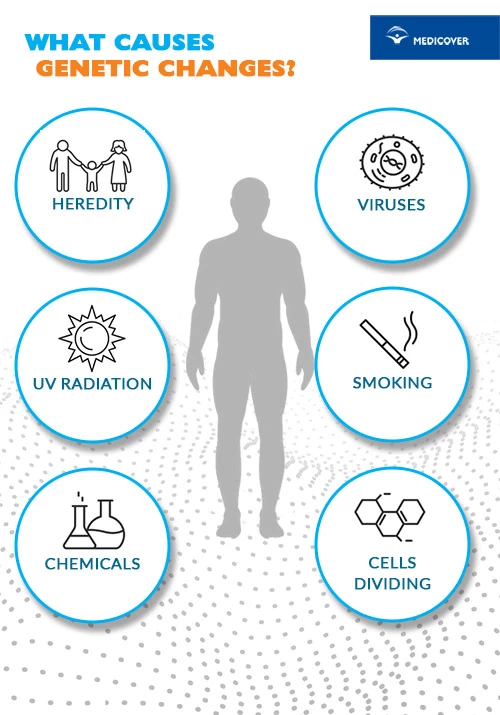
The genetic changes that cause cancer can be inherited or result from certain environmental exposures, such as exposure to carcinogens such as chemicals in tobacco smoke, UV radiation, or human papillomavirus (HPV) infection. They can also occur due to random errors during cell division.
Genetic mutations cause uncontrolled growth of cells and, consequently, the development of a malignant tumor. They can be spontaneous, i.e. they are formed spontaneously, most often during DNA replication during natural processes, such as cell division. physical (e.g. radiation, temperature), chemical (e.g. certain toxic substances) or biological (viruses) factors.
Mutations are divided into point (gene) mutations and mutations of longer DNA sequences and chromosomal mutations (chromosome aberrations).
Mutations can occur in both germ cells and somatic cells. In the first case, they are inherited (passed on to offspring) and can cause genetic diseases. In the second, they can lead to neoplastic transformation or affect the function of proteins, causing them to lose their activity or acquire unusual functions. However, they only apply to the person in whom they occurred.
Changes in DNA, whether caused by an accidental mistake or a carcinogen, can occur throughout our lives and even during fetal development. Most genetic changes are not harmful in themselves or are eliminated or compensated by repair mechanisms - they correct DNA damage that, for example, naturally occurs during cell division. to uncontrolled divisions that lead to the formation of cancer. Healthy cells can also turn into cancerous cells when genetic changes have accumulated over the years. Changes in genes that occur at any time during an organism's life are referred to as somatic (or acquired) mutations. Somatic mutations, which accumulate over a lifetime, account for 90-95% of all cancer cases.
Is cancer hereditary?
Cancer itself is not inherited, i.e. passed from parents to children, but a genetic change that increases the risk of cancer can be inherited. Some types of cancer, mainly breast, ovarian, colorectal and prostate cancer, are strongly linked to genes and may run in families.
For example, if a parent passes on a mutated BRCA1 or BRCA2 gene to their child, their child is at increased risk of developing breast cancer and several other cancers.
Up to 10% of all cancers can be caused by inherited genetic changes.
Inheriting a genetic change associated with cancer does not mean that you will definitely develop the disease. It only means that the risk of developing cancer is increased and such a person should be subject to special oncological observation. Awareness of the genetic load allows to take appropriate preventive measures and motivates to regular screening tests, which enable early detection of neoplastic changes.
Family members may have a higher than average risk of developing a certain type or types of cancer. Inheritance is usually related to closely related people.
In some cases, there is a tendency to develop cancer early in life or other non-cancerous conditions.
For example, familial adenomatous polyposis (FAP) is a familial cancer syndrome caused by certain inherited changes in the APC gene. People with FAP have a very high chance of developing colorectal cancer at a young age, and are also at risk of developing other types of cancer.
But not all cancers that seem to run in families are caused by passed down mutations. A shared environment or habits, such as exposure to air pollution or tobacco use, can cause the same type of cancer to develop among family members.
The inheritance of a predisposition to the development of cancer concerns, among others:
- breast cancer,
- ovarian cancer,
- colorectal cancer,
- eyeball cancer,
- kidney cancer,
- neurofibromatosis,
- melanoma.
Some mutated genes may increase the risk of breast cancer by 10-fold, and ovarian and colorectal cancer by up to 40-fold.
Genetic counseling and testing
Counseling and genetic testing make it possible to determine whether a person who does not show symptoms of cancer has inherited a mutation that increases the likelihood of developing cancer. Thanks to this, it is possible to prevent the development of cancer and take appropriate preventive measures.
Cancer genetic testing uses the latest technological advances to study the human genome, our complete genetic material (DNA). Scientists are looking for errors responsible for the formation of diseases in it. Once they identify the changes that cause cancer, they can better understand the molecular basis of cancer development, metastasis and drug resistance.
Through research into the genomic changes associated with cancer, drugs have been developed to fight the disease. They are divided into 3 groups:
- drugs that inhibit the activity of enzymes that trigger the abnormal growth and survival of cancer cells,
- medicines that block abnormal expression of genes characteristic of cancer cells,
- drugs that block molecular signaling pathways important for cancer cells.
These so-called Targeted therapies primarily target characteristics of cancer cells that are different from normal cells in the body. This makes them less toxic to patients compared to other treatments such as chemotherapy and radiation, which can kill normal cells.
Should everyone get genetic testing to determine their cancer risk?
Genetic tests are intended primarily for people without symptoms indicating cancer, but coming from genetic risk families, i.e. those in which a specific type of cancer has been diagnosed among close relatives (e.g. grandmother, mother, sister). These tests should be performed in selected clinical situations by professional laboratories. In special cases, it is recommended to consult a clinical geneticist. Your doctor can help you decide if you should have these tests based on your family medical history, and will explain the results once they are done. In addition, it will determine the search for genetic changes in a specific panel of genes characteristic of a given disease.
| Genetic tests can be helpful for people with a family history of cancer (e.g. breast cancer, ovarian cancer) in making decisions about screening tests. |
Genetic testing for cancer risk mutations is usually done with a blood sample or oral swab (saliva or epithelial cells from inside the cheek).
What genetic tests for cancer are currently being performed?
Currently, so-called tumor panels are often made. These are extensive genetic tests based on the sequencing of several genes to identify mutations associated with a given type of cancer or responsible for an increased risk of cancers typical for a given sex.
Genetic testing for breast and ovarian cancer
Breast cancer, also called nipple cancer, is the most common malignant tumor in women in Poland.
The incidence of breast and ovarian cancer is associated with BRCA1, BRCA2, PALB2, CHEK2, and NBN gene mutations.
Normally, the BRCA1 and BRCA2 genes protect against certain cancers because they are responsible for repairing damaged DNA. But some mutations prevent them from working properly, so inheriting one of them puts you at greater risk of breast, ovarian and other cancers.
Mutations in the BRCA1 and/or BRCA2 genes are usually spontaneous and can be inherited from both parents - if either the mother or father has a BRCA1 or BRCA2 mutation, the child has a 50% chance of being born. chance of inheriting it. Everyone has two copies of the BRCA1 and BRCA2 genes: one copy inherited from the mother and one from the father. Even if a person inherits a BRCA1 or BRCA2 mutation from one parent, they still have a "normal" copy of the BRCA1 or BRCA2 gene from the other. Cancer risk occurs if two mutations occur and there is no longer a BRCA1 or BRCA2 gene that is working properly. Of course, not everyone who inherits a BRCA1 or BRCA2 mutation will develop breast or ovarian cancer.
Type of cancer | Gene mutation risk | |
BRCA1 | BRCA2 | |
Breast cancer | 57-84 pct. | 41-84 pct. |
Ovarian cancer | 24-54 pct. | 11-27 pct. |
Prostate cancer | 16-20 pct | 20-34 pct. |
Breast cancer in men | 4 pct. | 4-7 pct. |
Pancreatic cancer | 3 pct. | 5-7 pct. |
Carriers of the mutation responsible for breast cancer undergo regular imaging tests - ultrasound and/or mammography (depending on the age group).
Genetic tests are especially recommended for women with a family history of:
- colorectal cancer,
- pancreatic cancer,
- breast cancer,
- ovarian cancer,
- prostate cancer,
- endometrial cancer,
- kidney cancer,
- thyroid cancer,
- stomach cancer,
- melanoma.
They are also recommended to those people whose closest relatives have confirmed the presence of any gene mutation that increases the risk of developing cancer.
Tests are also recommended to those who want to check their genetic predisposition to develop a given cancer.
Genetic testing for prostate cancer
An increased risk of prostate cancer is associated with mutations in the BRCA1, BRCA2, NBS1, HOXB13 and CHEK2 genes.
Researchers estimate that the risk of developing prostate cancer is 12 percent. in a person without a genetic load. In men with a congenital mutation, which most often occurs in the BRCA1 gene, it can be even more than three times higher.
Genetic tests detecting mutations associated with an increased risk of prostate cancer are recommended especially for people with a family history of:
- cases of prostate cancer,
- cases of ovarian, breast, pancreatic or colon cancer,
- mutations in the BRCA1, CHEK2 or NBS1 genes in relatives.
Genetic testing for colorectal cancer
As much as 82 percent of people with colorectal cancer have an identified genetic predisposition.
As part of genetic testing, as many as 25 genes that increase the risk of the disease are analyzed.
Patients diagnosed with a genetic predisposition towards bowel cancer are provided with an individual plan of prevention and early detection of colorectal cancer. As part of this prophylaxis, the frequency of colonoscopy and fecal occult blood tests is modified.
Genetic testing and the HPV virus
Screening: liquid cytology and HPV-DNA testing are used for the early detection of precancerous lesions and cervical cancer. The HPV virus is the main cause of cervical cancer. It is also dangerous for men, in whom it causes anal and penile cancer. HPV can also affect the oral cavity (as a result of unprotected oral intercourse) and is responsible for throat and mouth cancers.
Cytology with HPV genotyping allows you to diagnose HPV infection and determine whether it is a high-oncogenic type, i.e. one that is particularly conducive to the development of cervical cancer. As a screening test, it is recommended for patients over 30 years of age. and can be performed once every 5 years. Based on the type of virus, the risk of developing cancer is determined. This allows, if necessary, to decide on the implementation of appropriate prophylaxis, which consists in regular cytology tests (more often than for the general population).
Summary
|
Sources:
https://www.cdc.gov/genomics/disease/breast_ovarian_cancer/genes_hboc.htm (access on: 15/11/2022)
https://www.cancer.gov/about-cancer/causes-prevention/genetics (access on: 15/11/2022)
https://www.zwrotnikraka.pl/badania-genetyczne-na-raka/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9084432/#:~:text=BRCA1%20and%20BRCA2%20PVs%20are%20associated%20with%20increased,associations%20were%20found%20with% 20risks%20of%20other%20cancers.


